Çocuk Kalp Hastalıkları ve Cerrahisi (Pediatric Heart Diseases and Cardiac Surgery)
Çocuk Kalp Cerrahisi Platformu (Platform for Pediatric Heart Surgery)
Pediatrik Kalp Hastalıkları ve Cerrahisi
Pediatric Heart Diseases and Cardiac Surgery
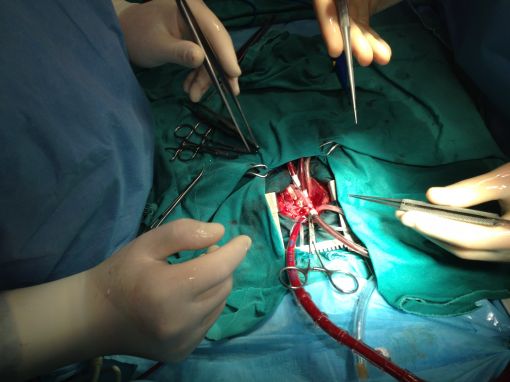
Arterial Switch ameliyatı
Arterial Switch Procedure (Jatene)
for D-Transposition of the Great Arteries (TGA)
Simple TGA'lı bir yenidoğana uyguladığımız Arterial Switch (Jatene) operasyonu

Op.Dr.Bugra HARMANDAR

Pathophysiology
D-Transposition of the great vessels is a
congenital cardiac anomaly in which the aorta arises from the right ventricle,
and the pulmonary artery arises from the left ventricle. Desaturated venous
blood returning from the peripheral tissue is pumped back to the systemic
circulation and oxygen rich pulmonary venous blood is pumped back to the
pulmonary artery. Patients present with cyanosis. Patients with transposition
of the great vessels must have a communication between the systemic circulation
and the pulmonary circulation to be consistent with life. Ideally, these
patients will have a patent ductus arteriosus and an atrial septal defect.
These work together to allow blood to shunt from the left atrium to the right
atrium allowing oxygenated blood to enter the systemic circulation. Intravenous
infusion of prostaglandin E1 will usually open the ductus arteriosus and a
bedside balloon atrial septostomy is performed to create a communication
between the atria.
The arterial switch procedure is usually performed in the first two weeks of
life. Following the early newborn period, left ventricular strength will begin
to regress as pulmonary vascular resistance falls. It is for this reason that
the operation is performed in the newborn period while the left ventricle
remains adequately prepared to support the systemic circulation.
Surgical Technique
The arterial switch procedure requires cardiopulmonary bypass and aortic cross clamping. Following aortic cross clamping, the ascending aorta and main pulmonary artery are transected. The left and right coronary artery ostia are visualized and excised from the aortic root with adjacent aortic wall as "buttons". The coronary artery buttons are then shifted posteriorly and implanted into the facing sinuses of the main pulmonary artery root. Next, the distal pulmonary artery and its branches are brought forward (LeCompte maneuver), and the distal aorta is moved posteriorly. The distal aorta is now anastomosed to the "new" aortic root. Reconstruction of the pulmonary artery is undertaken next, utilizing a patch of cryopreserved pulmonary artery homograft. Closure of the atrial septal defect completes the arterial switch repair. Transesophageal echocardiography is utilized to help assess adequacy of repair. Delayed sternal closure is sometimes required following surgery.
Postoperative Considerations
The postoperative course following arterial switch surgery can be variable. This is an extensive operation. Lengthy great vessel suture lines predispose these patients to postoperative bleeding. Myocardial dysfunction is sometimes encountered and may require moderate dose inotropic support. Patients who present late, following regression of neonatal pulmonary vascular resistance, are more likely to encounter left ventricular dysfunction. Invasive monitors utilized following surgery include arterial, central venous, and left atrial catheters. An oximetric catheter is utilized to monitor cardiac output. Vasoactive infusions required for hemodynamic management might include dopamine or dobutamine, epinephrine, milrinone, nitroprusside, phenoxybenzamine, and nitroglycerin. Cardiac arrhythmias are a rarely encountered postoperative complication. Intracardiac pressures following arterial switch surgery should be normal. Arterial oxygen saturation should be normal. Length of hospital stay following repair averages one to two weeks.




Yorumlar - Yorum Yaz